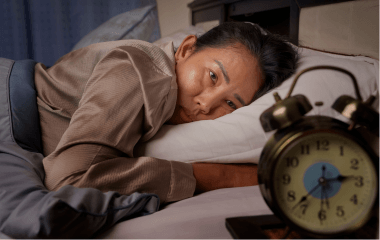
DARIEN, IL – While infections and hospitalizations from the COVID-19 virus are expected to rise during the fall and winter respiratory virus season, a new study suggests that sleep duration modulates the relationship between pre-existing medical conditions and long COVID.
Compared with individuals who had no pre-existing conditions and an average sleep duration of 6 to 9 hours per night, the risk of long COVID was three times higher in people who had pre-existing conditions and a short sleep duration of less than 6 hours per night (adjusted odds ratio = 2.95). In contrast, the risk of long COVID in people with pre-existing conditions was only 1.8 times higher among people with an average nightly sleep duration (adjusted odds ratio = 1.84). These analyses were adjusted for potential confounders including sex, age, body mass index, vaccination status, and ethnicity.
“Habitual short nighttime sleep duration exacerbated the risk of long COVID in individuals with pre-existing conditions,” said senior author Dr. Frances Chung, the ResMed chair in anesthesia, sleep, and perioperative medicine research at University Health Network and professor in the University of Toronto Department of Anesthesiology and Pain Medicine. “Based on its proven adjuvant role in immunity, habitual sleep duration may alter the risk for developing long COVID.”
The study was published as an accepted paper Oct. 3 in the Journal of Clinical Sleep Medicine, the official publication of the American Academy of Sleep Medicine.
According to the Centers for Disease Control and Prevention, some people who have been infected with the COVID-19 virus can experience long-term effects, known as long COVID. Symptoms may include tiredness or fatigue, difficulty breathing or shortness of breath, sleep problems, and difficulty thinking or concentrating (sometimes referred to as “brain fog”).
The study analyzed data from an online survey of 13,461 adults from 16 countries. Participants were categorized as COVID-19 cases if they indicated that they had been infected by the COVID-19 virus and had tested positive for COVID-19 infection. Pre-existing medical conditions were defined as medical conditions existing prior to a COVID-19 infection. Long COVID was defined as having a history of COVID-19 infection with at least one symptom lasting for more than three months according to the definition of the World Health Organization. Participants reported how many hours per night they sleep on average.
Among the 13,461 survey participants who answered the specific questions about COVID-19 diagnosis, there were 2,508 individuals who reported having a COVID-19 infection, and 20% reported at least one long COVID symptom. Of the 1,505 participants with long COVID who also reported their sleep duration and pre-existing condition status, 945 had pre-existing conditions, and 560 had none; and 121 (8%) were short sleepers, 1,257 (83.5%) had an average sleep duration, and 127 (84%) had a long nightly sleep duration of more than 9 hours.
According to Chung, sleep duration is a target for interventions to reduce the risk of long COVID.
“Restoring nighttime sleep to average duration represents a potentially modifiable behavioral factor to lower the odds of long COVID for at-risk patients,” she said.
The authors noted that more research is needed to understand the pathophysiology of long COVID.
###
To request a copy of the study, “Habitual short sleepers with pre-existing medical conditions are at higher risk of Long COVID,” or to arrange an interview with Dr. Chung or an AASM spokesperson, please contact the AASM at 630-737-9700 or media@aasm.org. Accepted papers, which are published online prior to their final inclusion in an issue, are not embargoed. The study will be published in an upcoming issue of the Journal of Clinical Sleep Medicine.
About the American Academy of Sleep Medicine
Established in 1975, the AASM advances sleep care and enhances sleep health to improve lives. The AASM has a combined membership of 12,000 accredited sleep centers and individuals, including physicians, scientists and other health care professionals who care for patients with sleep disorders. As the leader in the sleep field, the AASM sets standards and promotes excellence in sleep medicine, health care, education and research.