On March 17, the Centers for Medicare & Medicaid Services announced expanded Medicare telemedicine coverage that will enable beneficiaries to receive a wider range of health care services from their doctors without having to travel to a health care facility. Medicare will temporarily pay clinicians to provide telemedicine services for beneficiaries residing across the entire country.
This temporary change will help ensure Medicare beneficiaries, who are at a higher risk for COVID-19, are able to visit with their doctor from their home, without having to go to a doctor’s office or hospital, which puts themselves or others at risk. CMS indicates that for the duration of the COVID-19 public health emergency, Medicare will make payment for telemedicine services furnished to patients in all areas of the country and in all settings.
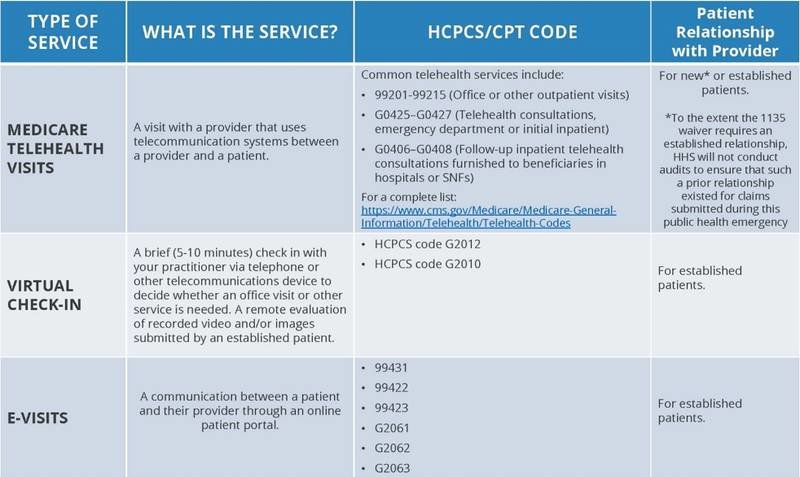
These visits are considered the same as in-person visits and are paid under the Physician Fee Schedule at the same rate as regular, in-person visits. Clinicians can bill immediately for dates of service starting March 6, 2020. In addition to these virtual visits, the expanded coverage also includes virtual check-ins and e-visits. During this public health emergency, CMS reports that it will not enforce any requirement that the patient have a prior established relationship with a particular practitioner.
The HHS Office for Civil Rights also announced that it will waive potential HIPAA penalties for good faith use of telemedicine during the nationwide public health emergency due to COVID-19. This change will allow covered health care providers to use everyday communications technologies to offer telemedicine. Providers can use any non-public facing remote communication product that is available to communicate with patients (including Apple FaceTime, Facebook Messenger video chat, Google Hangouts video, or Skype). However, Facebook Live, Twitch, TikTok, and similar video communication applications that are public facing should not be used in the provision of telemedicine.
Get complete details:
- CMS Announcement: President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak
- CMS Fact Sheet: Medicare Telemedicine Health Care Provider
- CMS FAQs: Medicare Telehealth Frequently Asked Questions
- CMS: General Provider Telehealth and Telemedicine Tool Kit
- HHS Notice: Notification of Enforcement Discretion for telehealth remote communications during the COVID-19 nationwide public health emergency
- VIDEO: Introducing Telemedicine Into Your Sleep Practice
Learn more about telemedicine. Send coding questions to the AASM at coding@aasm.org.
**UPDATE – March 30: Today CMS announced sweeping, temporary regulatory changes to help address the COVID-19 patient surge, including the elimination of requirements for face-to-face or in-person encounters. During this public health emergency, CMS will not enforce the clinical indications for coverage for CPAP for OSA, allowing Medicare to cover CPAP devices based on the clinician’s assessment of the patient. Read the fact sheet for physicians and other clinicians and the interim final rule.