On March 19 the American Medical Association (AMA) released the results of a physician survey showing widespread negative experiences with the implementation of prior authorization in the U.S. health care system.
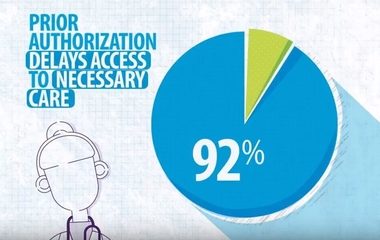
In a group of 1,000 physician respondents, 9 in 10 physicians report that current prior authorization programs are a detriment to achieving positive patient outcomes in clinical care. Additionally, nearly two-thirds of the surveyed physicians report waits of at least one business day for a prior authorization decision from their patient’s insurer, and just under 4 in 5 physicians agree that the prior authorization process at least sometimes results in a patient abandoning their treatment.
“The AMA survey illustrates a critical need to help patients have access to safe, timely, and affordable care, while reducing administrative burdens that take resources away from patient care,” AMA Chair-elect Dr. Jack Resnick Jr. said in a statement. “In response, the AMA has taken a leading role in convening organizations representing, pharmacists, medical groups, hospitals, and health insurers to take positive collaborative steps aimed at improving prior authorization processes for patients’ medical treatments.”
In September 2017, the AASM signed on to an AMA letter, Prior Authorization and Utilization Management Reform Principles, which suggests 21 common-sense measures for future prior authorization policy. This effort led to the Consensus Statement on Improving the Prior Authorization Process, a statement authored by the AMA, American Hospital Association, America’s Health Insurance Plans, American Pharmacists Association, the Blue Cross Blue Shield Association, and the Medical Group Management Association, which outlined five areas of agreement in future policy-making efforts:
- Selective application of prior authorization
- Prior authorization program review and volume adjustment
- Transparency and communication regarding prior authorization
- Continuity of patient care
- Automation to improve transparency and efficiency
Learn more about how the AMA is addressing prior authorization issues. For further discussion on prior authorization reform and advocacy, please contact AASM advocacy staff by phone at (630) 737-9700 or by email at policy@aasm.org.