In a Nov. 8 announcement, the Centers for Medicare and Medicaid Services (CMS) released data summarizing the year one payment adjustment results and highlighting the overall success of the Quality Payment Program (QPP).
In year one, more than one million clinicians who were eligible for the Merit-based Incentive Payment System (MIPS) qualified to receive a MIPS payment change. Of those, 95 percent reported data as either an individual, part of a group, or through an Alternative Payment Model (APM) and received a neutral payment adjustment or better, with only five percent earning a negative change. Under the APM track, 99,076 eligible clinicians earned Qualifying APM Participant (QP) status.
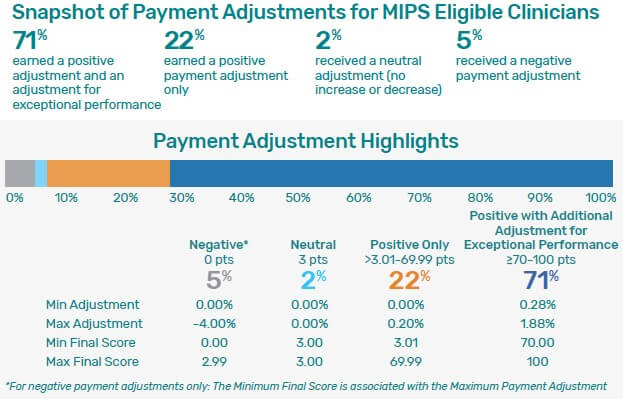
Results for year one are summarized below:
- 71% of MIPS eligible clinicians earned a positive adjustment and an adjustment for exceptional performance
- 22% earned a positive payment adjustment
- 2% earned a neutral adjustment, meaning there was no increase or decrease
- 5% earned a negative payment adjustment
According to the CMS announcement, “It is important to remember that the funds available for positive payment adjustments are limited by the budget neutrality requirements in MIPS, as established by law under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA).”
The overall national mean score for MIPS-eligible clinicians was 74.01 points, and the national median was 88.97 points.
- Clinicians participating in MIPS as individuals or groups received a mean score of 65.71 points and a median score of 83.04 points.
- Clinicians participating in MIPS through an APM received a mean score of 87.64 points and a median score of 91.67 points.
CMS credits the low performance threshold and the “pick your pace” program feature for providing flexibility and encouraging participation. It is expected that gradual increases in performance thresholds will significantly impact payments in the future.
Read more about the QPP year one performance results.