On July 1, 2025, the Centers for Medicare & Medicaid Services (CMS) released the 2023 Quality Payment Program (QPP) Experience Report. This document provides data specific to sleep medicine providers as it relates to Merit-based Incentive Payment System (MIPS) measures. Per the 2023 QPP experience report, 541,421 clinicians received a MIPS payment adjustment. This is down 13% from 2022.
2023 Final Scores by Participation Option. Participation option refers to the level at which data is collected and submitted to MIPS.*
| Participation Option | Mean Final Score | Median Final Score |
|---|---|---|
| Individual (45,044 MIPS eligible clinicians) |
56.16 | 75.00 |
| Group (375,400 MIPS eligible clinicians) |
82.87 | 82.91 |
| Subgroup (101 MIPS eligible clinicians) |
89.98 | 93.62 |
| Virtual Group (300 MIPS eligible clinicians) |
74.88 | 75.00 |
| APM Entity (120,576 MIPS eligible clinicians) |
94.24 | 94.31 |
*75 points are required to meet the performance threshold and is the minimum final score needed to avoid a negative payment adjustment.
2023 Final Scores by Participation Option – Sleep Medicine Providers Only.
| Participation Option | Mean Final Score | Median Final Score |
|---|---|---|
| Individual | 47.65 | 64.84 |
| Group | 81.23 | 81.31 |
| Subgroup | N/A | N/A |
| Virtual Group | N/A | N/A |
| APM Entity | 94.76 | 95.31 |
Of the 541,421 clinicians who received a MIPS payment adjustment, 415 were sleep medicine providers. 84.3% (350) of the sleep medicine providers received a positive payment adjustment.
MIPS Payment Adjustment Range – Sleep Medicine Providers Only.
| Payment Adjustment Range | 2023 |
|---|---|
| Positive Only (75.01-100 points) | 350 |
| Neutral (75 points) | 13 |
| Negative (18.76-74.99 points) | 36 |
| Max Negative (0-18.75 points) | 16 |
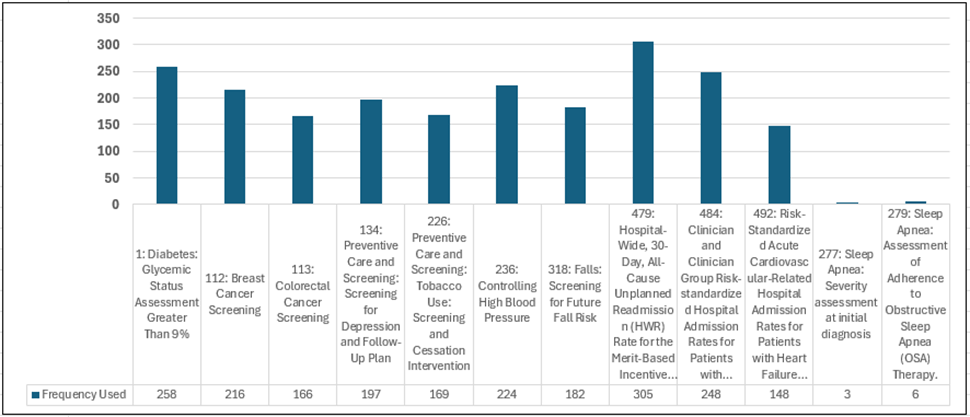
The graph below shows the top 10 measures contributing to sleep medicine providers quality performance along with the two AASM MIPS measures (277 & 279). The number shown indicates the frequency by which each specific measure was submitted for the MIPS quality final score.
Links to additional resources from CMS are provided below:
- 2023 QPP Participation and Performance Results At-a-Glance
- 2023 QPP Experience Report
- 2023 QPP Public Use File
- This file contains data at the TIN/NPI level. In accordance with CMS guidelines, information is suppressed for TIN/NPIs with fewer than 15 beneficiaries. As a result, the figures in the public use file may differ from those presented in the QPP experience report.
Questions regarding AASM MIPS measures should be directed to our registry team at registry@aasm.org.