How high is hypertension? Earlier this week a new clinical practice guideline for high blood pressure in adults was published by the American College of Cardiology (ACC) and the American Heart Association (AHA). It represents the first comprehensive hypertension guideline to be published in 14 years.
High Blood Pressure
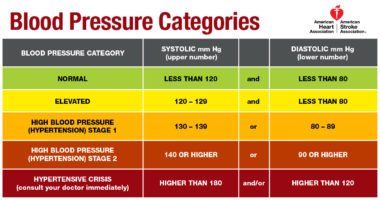
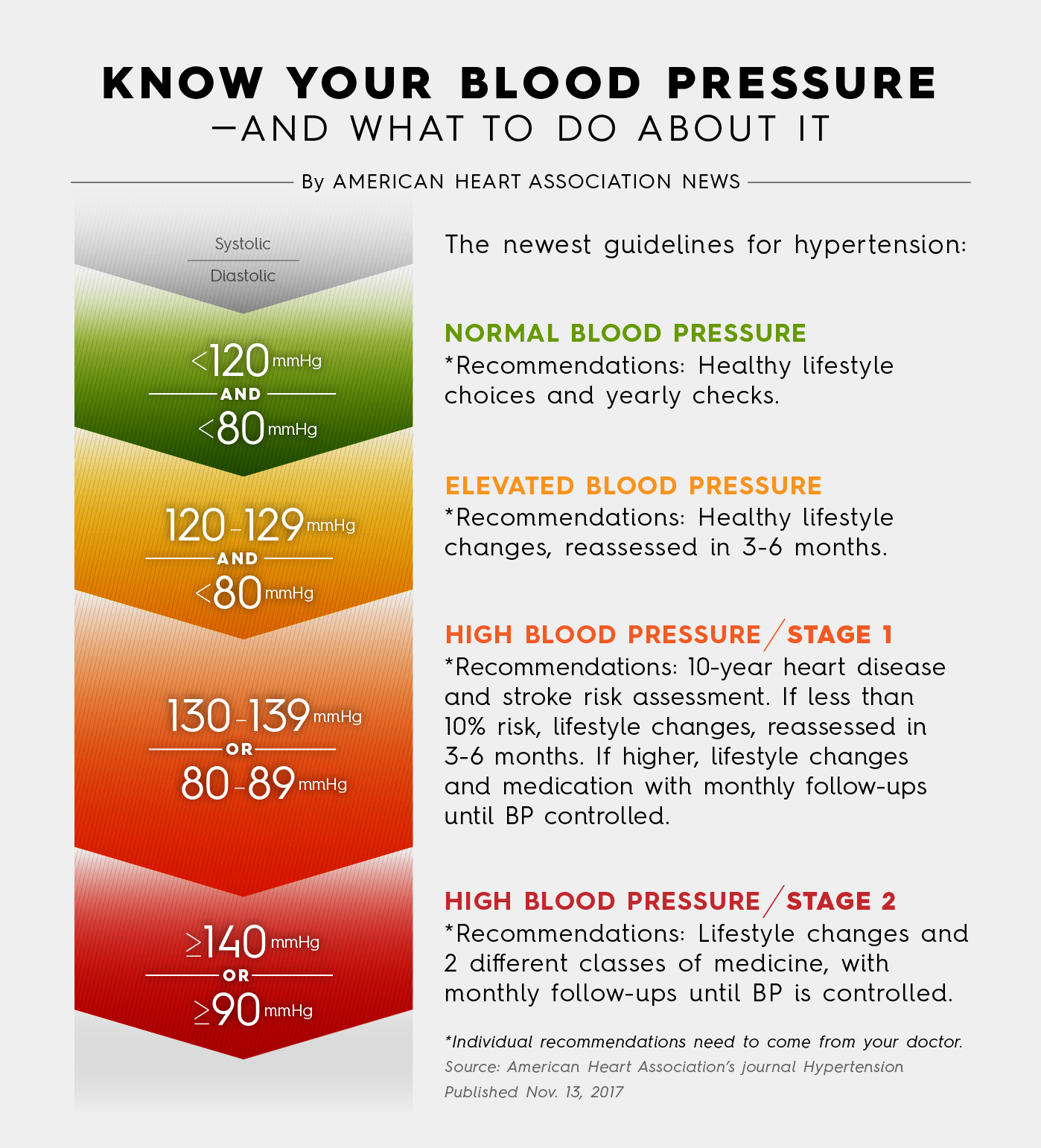
A blood pressure of less than 120/80 still will be considered normal, but levels at or above that, up to 129, will be called “elevated.” The guideline redefines hypertension as stage 1 (130/80 to 139/89 mm Hg) and stage 2 (140/90 mm Hg and higher), with different implications for treatment.
High blood pressure used to be defined as 140/90. A separate analysis estimates that the new guideline results in a substantial increase in the prevalence of hypertension, from 31.9% to 45.6%, with an estimated 103.3 million U.S. adults having hypertension according to the new definition.
The guideline recommends that people who are 65 years of age and older be treated to the same 130/80 goal as younger patients. However, a different guideline, published earlier this year by the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP), specifically addressed the pharmacologic treatment of hypertension in adults aged 60 years or older. It recommends that clinicians initiate treatment in adults aged 60 years or older with systolic blood pressure persistently at or above 150 mm Hg to achieve a target systolic blood pressure of less than 150 mm Hg.
Obstructive Sleep Apnea
The new guideline describes obstructive sleep apnea as a “relatively fixed” cardiovascular disease risk factor in patients with hypertension. It also lists obstructive sleep apnea as a cause of secondary hypertension, with resistant hypertension being one of the clinical indications.
However, the guideline also recommends that in adults with hypertension and obstructive sleep apnea, the effectiveness of continuous positive airway pressure (CPAP) to reduce blood pressure is not well established. It notes that studies of the effects of CPAP on blood pressure have demonstrated only small effects on blood pressure, with results dependent on patient adherence to CPAP, severity of obstructive sleep apnea, and presence of daytime sleepiness in study participants. The guideline further states that it has been hypothesized that treatment with CPAP may have more pronounced effects on blood pressure reduction in resistant hypertension.