The Centers for Medicare & Medicaid Services released the CY 2026 Medicare physician fee schedule (MPFS) final rule on Oct. 31, 2025. AASM submitted a comprehensive comment letter to CMS outlining priority policy changes to protect patient access to sleep medicine services, ensure accurate valuation of sleep procedures, and minimize payment instability.
The final rule includes several significant policy changes that impact sleep physicians, sleep technologists and sleep facilities. Although CMS finalized many broad policies with system-wide effects, sleep-specific issues — including RVU valuation, efficiency adjustments, telehealth policies and indirect PE methodology — remain central to the 2026 payment landscape. Key themes for sleep medicine are outlined below.
Physician Payment
The AASM continues to advocate for Medicare reform through outreach to Congressional leaders both individually and in collaboration with other medical specialty societies and organizations. In response to these efforts, CMS finalized a 3.26% increase in the conversion factor for most physicians. Specifically, for clinicians who qualify as a qualifying APM participant (QP) in an advanced alternative payment model (APM), the agency finalized a conversion factor of $33.57, and for clinicians who do not qualify as a QP, the agency finalized a conversion factor of $33.40. While this appears to be a considerable increase, as shown in Table 1, it will be offset by a newly established efficiency adjustment and changes to the practice expense (PE) methodology.
See Table 1.
Table 1. Trends in the Medicare Conversion Factor
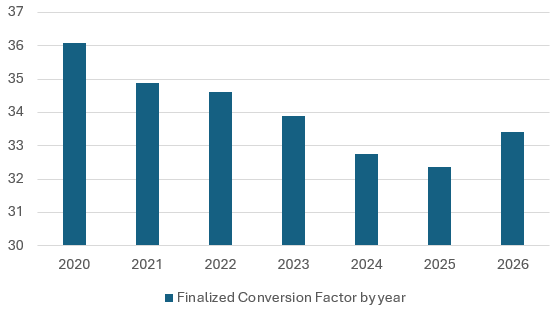
*The 2026 conversion factor included in Table 1 is the non-APM-eligible conversion factor.
Efficiency adjustment
As of 2026, there will be a -2.5% efficiency adjustment applied to work RVUs for nearly all non-time–based services. AASM opposed the efficiency adjustment, citing a lack of transparency and a disproportionate effect on cognitive specialties and diagnostic services. CMS finalized it largely unchanged, exempting time-based codes, including E/M office visits, telehealth-listed codes, maternity care, and the new 2026 codes. Nearly all sleep testing codes and PAP therapy management codes will be subject to the -2.5% cut.
Practice expense methodology change
CMS finalized a major shift in indirect practice expense (PE) for facility and non-facility settings. CMS reduced indirect PE RVUs for facility-based services by -7%, citing duplication of costs in hospital-owned practices and increased indirect PE RVUs for non-facility-based services by +4%. Polysomnography performed in hospital-based facilities may be subject to payment reductions, while non-facility sleep centers may see modest positive effects.
CMS also finalized maintaining and clarifying the existing site-of-service framework that continues to produce payment differentials between facility and non-facility settings and discussed approaches to recognize settings with different resource patterns. CMS reiterated that many professional services still have a facility vs. non-facility differential under the physician fee schedule and explained its approach to accounting for direct vs. indirect practice expenses in those settings. Sleep clinicians who provide services in ASCs, hospital-based labs or physician offices will continue to see different Medicare payments for the same CPT codes depending on the place of service.
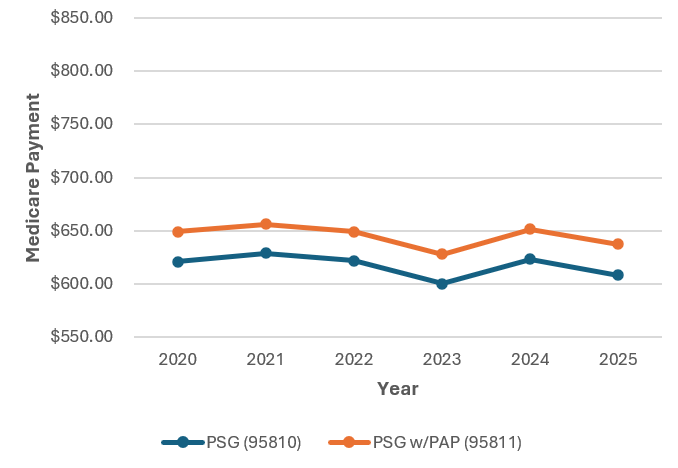
Note the trends in Medicare reimbursement for both unattended and attended (in-lab) sleep studies in Tables 2 and 3. See Tables 2 and 3.
Table 2. Trends in Medicare reimbursement for unattended sleep studies
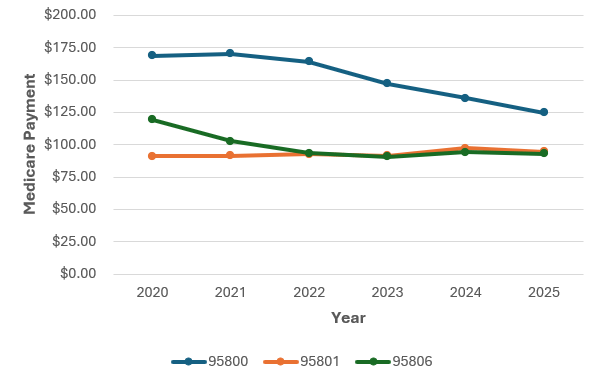
Table 3. Trends in Medicare reimbursement for attended (in-lab) sleep studies
Payment and RVU Comparisons
The AASM national payment and RVU comparison documents have been updated and are accessible via the links below.
- Sleep Medicine Payment and RVU Comparison
- Evaluation and Management Payment and RVU Comparison
- Telemedicine Payment and RVU Comparison
Determination of professional liability (PLI) RVUs
CMS finalized its proposed methodology for calculating malpractice PLI RVUs using updated state insurer filings, a specialty-weighted approach, and a stabilized/improved imputation methodology. The agency will update PLI RVUs at least every three years. The PLI RVU component is a small share of the total RVUs for each code but can marginally alter reimbursements.
Use of the physician practice information (PPI) survey to update PE inputs and the Medicare economic index
CMS declined to incorporate producer price index (PPI) survey data into its methodology for updating practice expense (PE) inputs and the Medicare economic index (MEI). Medical specialty societies, including the American Medical Association and AASM, urged CMS to adopt PPI-based updates because these data better reflect current inflationary pressures on equipment, supplies and clinical labor. CMS acknowledged the societies’ concerns but stated that additional methodological development and budget-neutrality modeling before it could be proposed in future rulemaking. As a result, CMS chose to maintain its existing cost-input methodologies and will continue to rely on vendor-sourced equipment pricing and internal MEI modeling. The continued use of outdated PE inputs contributes to persistent underpayment for sleep services across settings.
Potentially misvalued codes
RUC progress in identifying and reviewing potentially misvalued codes
CMS reaffirmed its statutory obligation to identify, review and adjust potentially misvalued codes but reiterated that while the AMA RUC remains a core source of recommendations for code valuation, it is not the sole authority on valuation, particularly for work RVUs, time values and direct practice expense inputs. CMS may also use Medicare claims data, empirical time data, public comments, published literature and its own internal analyses.
Neurostimulator pulse generator analysis codes (95970, 95976, 95977)
The neurostimulator pulse generator analysis codes were identified as potentially misvalued due to perceptions of inaccurate PE inputs, incorrectly attributed physician work, and a change in service mix. CMS does not consider codes 95970, 95976, and 95977 to be potentially misvalued. However, the agency welcomes additional data for future consideration, including detailed survey data, time and intensity analyses, updated PE documentation, input from specialties, and evidence of changes in technology or workflow. CMS acknowledged the possibility of a future review if more complete or compelling evidence is submitted to support the nomination.
Telehealth
Virtual direct supervision
After ongoing AASM advocacy, CMS finalized permanent virtual direct supervision, removal of frequency limits for inpatient and nursing facility telehealth visits, and continuation of key flexibilities. This supports sleep physicians who supervise home sleep apnea testing (HSAT), provide remote follow-up visits, and oversee advanced practice providers (APPs).
Provider enrollment and address flexibility
CMS acknowledged the prior flexibility that allowed distant-site telehealth practitioners to use their enrolled practice location (rather than home address) when furnishing telehealth from home, which had been previously extended through Dec. 31, 2025. In the final rule, CMS did not finalize a blanket requirement that would require all providers to publish or publicly display their home address. Therefore, providers with a physical practice location may continue to use the practice location for telehealth claims rather than their home address. Those practicing solely from home may enroll using their home address, and CMS will accept street address details from public provider directories when marked “home office for administrative/telehealth use only.” CMS will continue to publish operational guidance and frequently asked questions (FAQs) to provide updates on this issue.
Frequency limitations
CMS permanently removed the specific telehealth frequency limitations that previously capped how often certain subsequent inpatient visits, subsequent nursing facility visits, and critical care consultation services could be furnished via telehealth. Instead of fixed numeric caps, CMS finalized that clinicians should use their professional judgment to determine telehealth visit frequency on a case-by-case basis. Data collected during the COVID-19 public health emergency showed that telehealth flexibilities helped maintain access without widespread inappropriate use; commenters reported benefits to continuity of care. CMS emphasized the importance of clinician judgment and patient-specific safety considerations, rather than a blanket one-size-fits-all rule, but will consider implementing safeguards in the future if misuse is identified.
Remote physiologic monitoring (RPM) and remote therapeutic monitoring (RTM)
CMS finalized the use of ambulatory payment classifications (APCs) used in the outpatient prospective payment system (OPPS), a payment method by CMS for hospital outpatient services, relative weights to set PE RVUs for certain RPM and RTM codes, which AASM opposed due to misalignment with sleep monitoring. RPM codes commonly used in PAP adherence monitoring, oximetry data streams, etc., may face adjusted PE values that do not reflect actual practice costs.
Digital mental health therapeutics
CMS finalized measures to advance payment/coverage frameworks for digital mental health services and digital therapeutic tools, including separate discussions of digital mental health treatment services and how to integrate them into the physician fees schedule coding/care pathways. The final rule also clarifies the scope and emphasizes that CMS will continue to evaluate these tools with an emphasis on evidence and appropriate reimbursement. This highlights an opportunity to expand the integration of digital CBT-I and other behavioral sleep health apps into care and billing frameworks.
Facilitating diagnostic testing through telehealth
CMS finalized policies that continue to support telehealth as a mechanism to facilitate downstream diagnostic testing and clarified coding that supports remote evaluation/management and certain virtual services facilitating diagnostics. The agency listed telehealth-compatible codes and indicated support for coordination via telehealth where clinically appropriate. For sleep providers, this means that telehealth can be used to triage, order and interpret home sleep testing, provide pre-test instructions, and coordinate polysomnography scheduling without jeopardizing reimbursement. This will improve access, reduce delays in diagnosis, and lower downstream costs from untreated obstructive sleep apnea.
Evaluation and management visits
| G2211 | Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established) |
|---|
CMS finalized refinements to G2211, including permitting the add-on to be billed with home/residence E/M codes and refining the descriptor to include home/residence and office/outpatient services. CMS acknowledged utilization uncertainty and will continue to monitor this data going forward. Documentation will continue to be extremely important, specifically the longitudinal relationship rationale, when billing G2211.
The AASM will continue advocating for favorable changes to the physician fee schedule. Members may send questions on the physician fee schedule final rule to coding@aasm.org.