The Centers for Medicare & Medicaid Services (CMS) has posted the 2025 Medicare physician fee schedule final rule. This AASM analysis highlights changes in physician payment and sleep medicine reimbursement, specific Current Procedural Terminology (CPT) code updates, revisions to telehealth policies, and payment for dental and oral health services.
Physician Payment
The AASM continues to advocate for Medicare physician payment reform, as we encourage Congressional leaders to #RepairMedicare through AASM-led efforts as well as coordinated efforts with the American Medical Association (AMA) and other medical societies and organizations. These continued payer advocacy initiatives included an AASM response to the 2025 physician fee schedule proposed rule, in which we strongly opposed the proposed conversion factor. However, a reduced conversion factor of $32.3465 was finalized, setting in place a 2.83% reduction from 2024. See Table 1.
Table 1. Trends in the Medicare Conversion Factor
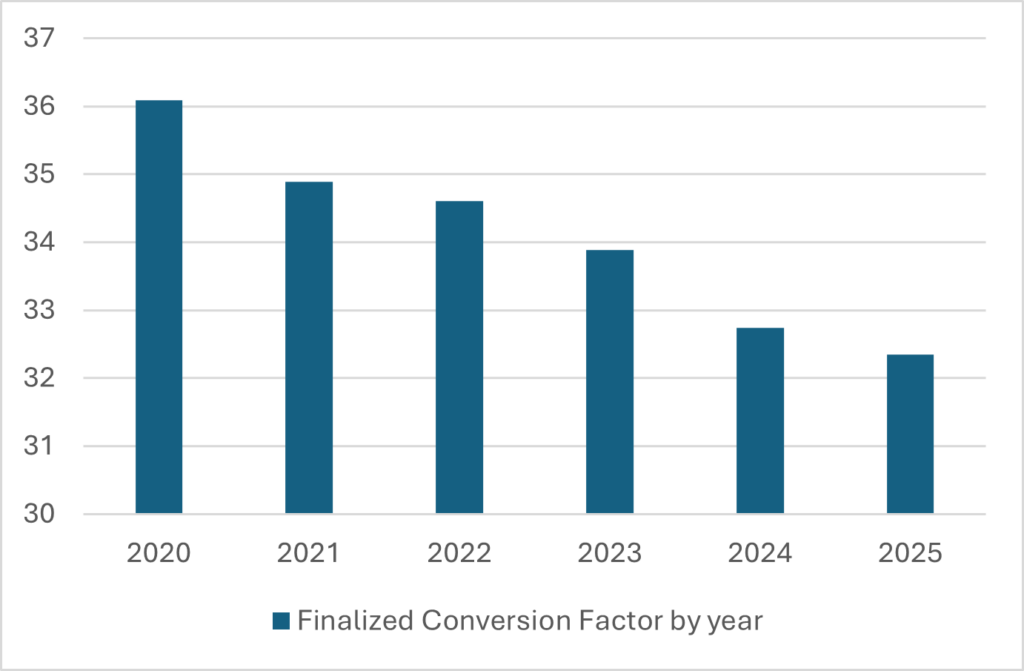
The AASM continues to advocate for an annual inflationary update to address the downward trend in physician reimbursements and encourages members to visit the AASM Action Center and join the current payer advocacy campaign to encourage Congressional leaders to sign on as co-sponsors of the Medicare Patient Access and Practice Stabilization Act of 2024 (H.R. 10073), which would give physicians a 4.73% payment increase in calendar year 2025. This payment increase would counteract the Medicare Economic Index (MEI) prediction that the cost of practicing medicine will increase by 3.6% in 2025.
The impact of the consistently decreasing conversion factor can be seen in the downward trend in reimbursements for sleep studies. See Table 2 and Table 3.
Table 2. Trends in Medicare Reimbursement for Unattended Sleep Studies

Table 3. Trends in Medicare Reimbursement for Attended Sleep Studies

Payment and RVU Comparisons
The AASM has put together updated national payment and relative value unit (RVU) comparison documents, which are available using the links below.
- Sleep Medicine Payment and RVU Comparison
- Evaluation and Management Payment and RVU Comparison
- Telemedicine Payment and RVU Comparison
Estimated Specialty Utilization
CMS also included information that parses out the aggregate estimated physician fee schedule allowed charges for each specialty based on 2023 utilization data and 2024 reimbursement rates, to demonstrate the potential impact of the finalized policies in this final rule. The agency predicted no combined impact for critical care, neurology, otolaryngology, or pulmonary disease. However, clinical psychology is predicted to have a combined impact of 3% across both non-facility and facility allowable charges, while pediatrics is predicted to have a combined impact of 1% in facility charges, and psychiatry is predicted to have a combined impact of 1% in non-facility charges. Sleep medicine is not included, as CMS categorizes it as a subspecialty.
Specific CPT Code Updates
Telemedicine E/M Office Visit codes (98000 – 98015)
The American Medical Association CPT Editorial Panel previously established 17 new telemedicine evaluation and management (E/M) office visit CPT codes, which were intended to capture audio-only services as well as audio-visual services. Once established, these codes were valued by the AMA/Specialty Society Relative Value Scale Update Committee (RUC). The RVU recommendations were then submitted to CMS for review and adoption. However, while CMS has finalized proposals to post the new codes and the recommended values, it did not adopt the codes for use in the Medicare program, as the agency does not believe that these services should be implemented for Medicare without new legislation being enacted. Instead, CMS acknowledged the deletion of the audio-only telephone services CPT codes, 99441 – 99443, and it committed to developing educational materials to assist with correct coding for audio-only vs. audio-video telemedicine services going forward.
Refinement of current policy for implementation of G2211
| G2211 | Visit complexity inherent to evaluation and management associated with medical care services that serve as the continuing focal point for all needed health care services and/or with medical care services that are part of ongoing care related to a patient’s single, serious condition or a complex condition. (Add-on code, list separately in addition to office/outpatient evaluation and management visit, new or established) |
|---|
While the Healthcare Common Procedure Coding System (HCPCS) code G2211 was implemented at the start of 2024, CMS originally prohibited reporting this code on the same day as preventive services, including annual wellness visits and vaccinations. However, CMS has refined the policy to allow payment for G2211 when E/M visits are provided by the same physician or qualified health care professional to the same patient on the same day as another serviced and billed with CPT modifier 25. The AASM encourages members to meticulously document when reporting G2211, as there tend to be audits after initial implementation of new, widely used CPT codes. Members are also encouraged to review the AASM’s Coding Quarterly article in Montage magazine regarding correct reporting of G2211.
Adoption of new code to replace G2012
| 98016 | Brief assessment (5–10 minutes) via synchronous communication technology at the request of an established patient for purposes of determining if a more extensive service (e.g., office visit) is indicated |
|---|
CMS finalized the adoption of CPT code 98016 in place of the HCPCS code G2012 for reporting a brief communication technology-based service, which has a non-facility payment rate of $15.85 and a facility payment rate of $14.56.
95800 as a potentially misvalued code
For two years in a row, CPT code 95800 was submitted as a potentially misvalued code, as the submitter indicated that the majority of sleep medicine providers have switched to using disposable equipment rather than reusable equipment for unattended diagnostic sleep studies reported via 95800. Again, AASM responded to this nomination by urging CMS to collect more data before making a final decision on updating the practice expense information for this code. The AASM is also working with the American Academy of Neurology (AAN), American Thoracic Society (ATS), and the American College of Chest Physicians (CHEST) to revise the unattended sleep testing codes so sleep medicine professionals can report codes accurately for new technologies and report diagnostic testing for multiple sleep disorders.
Revisions to Telehealth Policies
Without Congressional action, pre-pandemic geographic and location restrictions will be reinstated as of Jan. 1, 2025. This means that unless a Medicare patient lives or is located in a health professional shortage area, a rural census track, or a county outside of the metropolitan statistical area at the time of service, they will not be covered for telehealth services. Limitations on the scope of providers that can provide Medicare telehealth services will also be reinstated absent Congressional action.
The AASM is supporting the Telehealth Modernization Act of 2024 (H.R. 7623), which would permanently extend certain flexibilities and allow (1) rural health clinics and federally qualified health centers to serve as the distant site, (i.e., the location of the health care practitioner); (2) the home of a beneficiary to serve as the originating site (i.e., the location of the beneficiary) for all services (rather than for only certain services); and (3) all types of practitioners to furnish telehealth services as determined by CMS.
Additional telehealth policies finalized by CMS, as recommended by AASM, include:
- Providers may use two-way, real-time, audio-only communication for Medicare telehealth services furnished to a beneficiary in their home as long as the provider has video capabilities, regardless of whether the patient is capable or consents to using video technology.
- Direct supervision through real-time audio and visual interactive telecommunications (not audio-only) will continue to be allowed on qualifying services.
- Several behavioral and mental health services will be permanently offered under telehealth for Medicare patients beginning in 2025.
- Place of service (POS) codes will continue to have two telehealth designations:
- POS 02 Patient not in their home when telehealth services are rendered; or
- POS 10 Patient in their home when telehealth services are rendered.
- CMS will continue to allow physicians to list their practice address, rather than their home address, when performing Medicare services via telehealth from their home.
- Teaching physicians may continue to have a virtual presence in all teaching settings through Dec. 31, 2025, but only for Medicare telehealth services.
- CMS also finalized the adoption of three new digital mental health treatment codes, G0552 – G0554. The AASM asked that CMS modify the categorization of the codes to “digital health treatment” codes and to modify the code descriptors to allow for broader implementation and to include devices that do not automatically transmit data to providers. However, these modifications were not finalized. The code descriptors are provided below.
| HCPCS Code | Descriptor |
|---|---|
| G0552 | Supply of digital mental health treatment device and initial education and onboarding, per course of treatment that augments a behavioral therapy plan for furnishing a DMHT device |
| G0553 | First 20 minutes of monthly treatment management services directly related to use of the DMHT device |
| G0554 | Each additional 20 minutes of monthly treatment management services directly related to DMHT device |
Medicare payment for dental/oral health services
In 2023, CMS finalized that Medicare payment could be made when dental services are linked to, related, and integral to the clinical success of other Medicare covered services and has since added additional dental services to the list of Medicare covered services. In this 2025 final rule, the agency has expanded coverage and payment to include:
- Medically necessary diagnostic and treatment services to eliminate an oral or dental infection before or contemporaneously with Medicare-covered dialysis services for the treatment of end-stage renal disease (ESRD).
- Dental or oral examination in the inpatient or outpatient setting before or contemporaneously with Medicare-covered dialysis services for the treatment of ESRD.
CMS also finalized that the agency will delay implementation for both the ICD-10 codes as well as KX and GY administrative claims modifiers until July 1, 2025, to allow more time for comprehensive testing, reporting, and educational materials for providers, vendors, and payers.
Lastly, after reviewing responses from many medical organizations, including the AASM, in response to a request for information regarding services associated with furnishing an oral appliance for the treatment of obstructive sleep apnea (OSA), CMS did not make a final determination.
Members may send questions about the Medicare physician fee schedule final rule to coding@aasm.org.




