For a complete list of Quality and Health Policy 2024 Accomplishments, visit the 2024 Year in Review.
Unlock the Full Potential of Your Sleep Practice
Enhance your sleep practice’s efficiency and patient care with resources tailored specifically to the needs of sleep medicine professionals.
Exclusive Tools
Access the latest management resources and guides developed by sleep medicine experts.
Practice Optimization
Streamline operations, improve patient satisfaction, and boost financial performance.
Networking Opportunities
Streamline operations, improve patient satisfaction, and boost financial performance.
Equip Yourself with the Tools to Succeed
Take advantage of AASM’s comprehensive resources designed to enhance your practice, navigate complex regulations, and stay ahead of emerging trends. Whether it’s coding education, audit preparation, or new technologies, these tools empower you to make a meaningful impact in sleep medicine.

AASM Coding Education Program
The AASM Medical Coding Education Program (A-CEP) is the first and only online coding, insurance, and reimbursement education program developed specifically for the sleep center.

Medicare Audit Toolkit
A free member resource, the toolkit contains resources, tips, and information to increase knowledge of the overall audit process and assist member sleep facilities in preparing for audits and navigating the audit process.
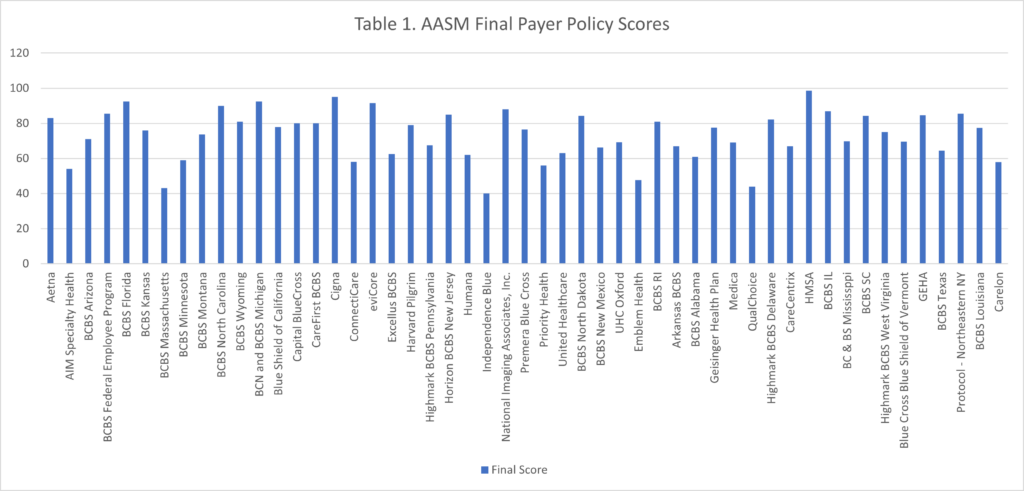
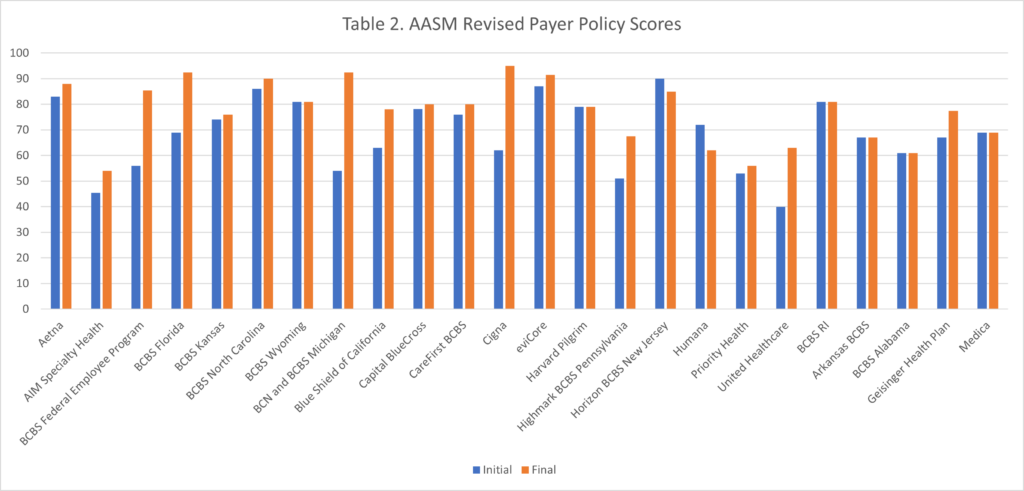
Payer Policy Scorecards
Payer policy scorecards were created to evaluate how effective payer policies are at establishing appropriate coverage for diagnostic sleep testing services. The intent of the scorecards is to encourage insurers to adopt evidence-based policies that support patient safety and delivery of high-quality care.
Webinar: The Role of the RUC Process in Physician Reimbursement
In this American Academy of Sleep Medicine webinar, Dr. Manaker assists AASM members in understanding the role of the RVS Update Committee (RUC) process in physician reimbursement, specifically highlighting the survey process and practice expense inputs and how they are incorporated into the Physician Fee Schedule.
Elevate Your Career in Sleep Medicine with AASM Membership
Join over 9,500 of your peers in discussions with your peers and industry leaders to expand your knowledge.
Exclusive Resources
Access cutting-edge research and clinical guidelines
Professional Development
Enhance your skills with conferences and courses
Community Engagement
Connect with experts and peers worldwide
Professional Advocacy
Shape the future of sleep medicine
Already a member? Log in to access exclusive resources