30
AASM Membership Sections Newsletter
■
Issue #6
American Academy
of Sleep Medicine
Final diagnosis:
Severe OSA with treatment emergent central
apneas.
1.
What is treatment emergent central sleep apnea
(TE-CSA) syndrome?
Treatment emergent central sleep apnea syndrome is characterized
by a central apnea index greater than 5/hour, and the central events
should comprise more than 50% of the total apneic events after
positive airway pressure (PAP) initiation. They occur in 18-20%
of patients that are newly initiated on PAP. It was previously
classified under “Complex Sleep Apnea Syndromes,” which was a
category used to describe individuals with both obstructive and
central apneas, mixed apnea and ataxic breathing. It is currently
classified under “Central Sleep Apnea (CSA) Syndromes,” along
with Cheyne-Stokes, CSA due to medical disorder without Cheyne-
Stokes, high altitude periodic breathing, CSA due to medication or
substance, primary CSA, primary CSA of infancy and primary CSA
of prematurity.
2.
Why does TE-CSA occur?
The exact mechanism by which these events occur is unclear. A
few of the current theories propose that this is a consequence of
patient-ventilator interaction. One theory postulates that pressure
from PAP activates stretch receptors in the lung and inhibits central
respiratory output by the Herring-Breuer inflation reflex. This has
been described as “pressure toxicity” in the past. Another thought
is that there is increased carbon dioxide washout with increased
leak at higher PAP pressures, leading to central apneas. However,
TE-CSAs have also been described in patients with obstructive
sleep apnea who have undergone tracheostomy in the era pre-dating
PAP. Therefore, the emergence of TE-CSA may be a characteristic
of subgroups of patients with obstructive sleep apnea. Patients with
sleep apnea have a high “loop gain.” Loop gain is an engineering
term used to describe the ventilator response for a given respiratory
disturbance. Individuals with sleep apnea have recurrent airway
occlusion during sleep. When this occlusion is resolved either
by PAP or tracheostomy, they are unable to rapidly adjust to this
decrease in airway resistance. Therefore, there may be a subgroup
of patients with obstructive sleep apnea, with an abnormal loop gain
that have periods of hyperventilation followed by central sleep apnea
after they are initiated on treatment for obstructive sleep apnea.
3.
What is the natural course of TE-CSA?
Current data suggests that TE-CSA may resolve by 8-12 weeks in
the majority of individuals. Specifically, in an observation study by
Dernaika and collegues (Chest, 2007), 23 out of 116 patients with
obstructive sleep apnea that were initiated on PAP had TE-CSA.
Note that patients with known systolic heart failure, stroke or opiate
use were excluded from this study. Fourteen patients returned for
repeat polysomnogram after 8-12 weeks. Twelve of the 14 patients
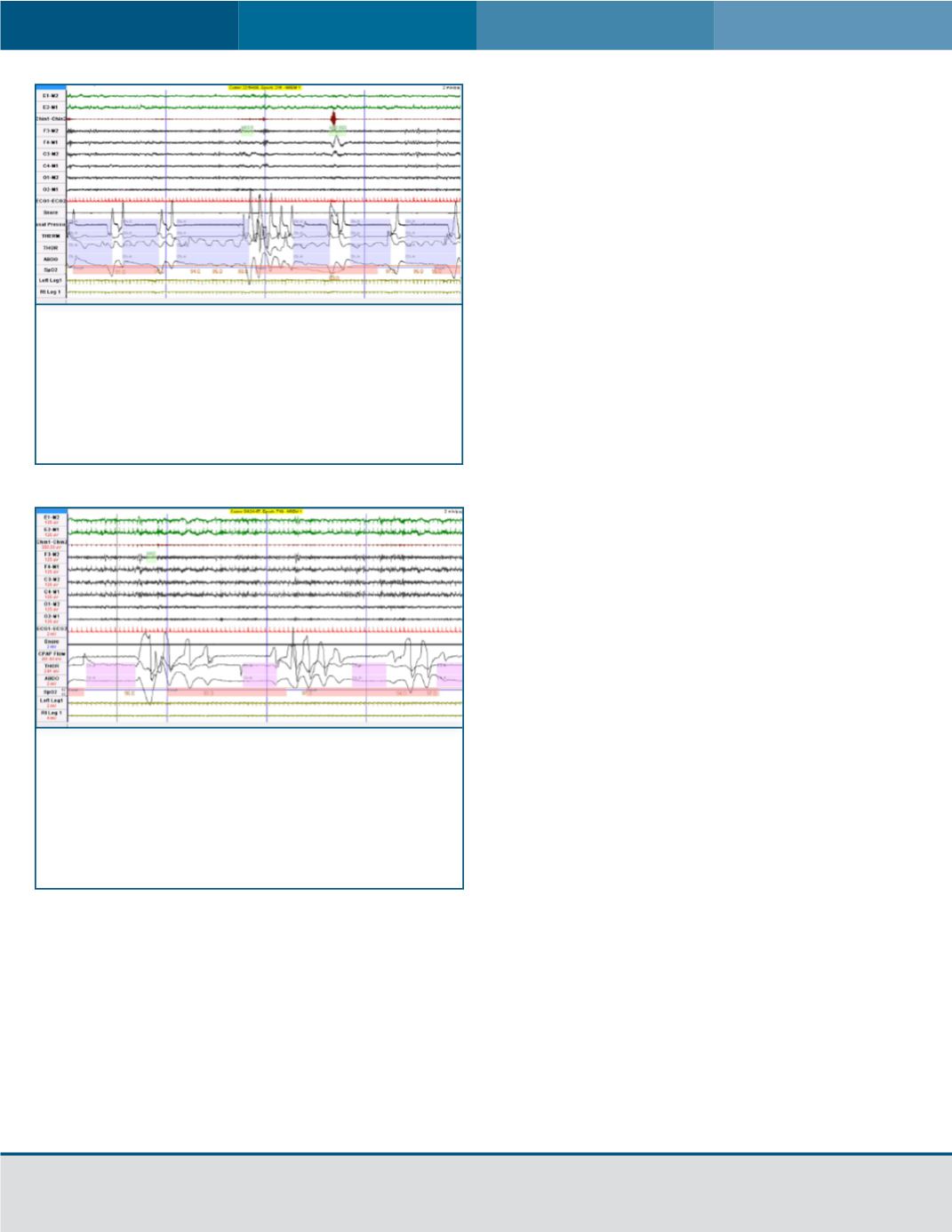
Figure 1:
Figure Image above depicts the diagnostic
portion of the polysomnogram in which there are
obstructive apneas, as demonstrated by a decrease in
the nasal pressure, despite respiratory effort noted on
the thoracic belt, with a concurrent desaturation noted
on the pulse oximeter.
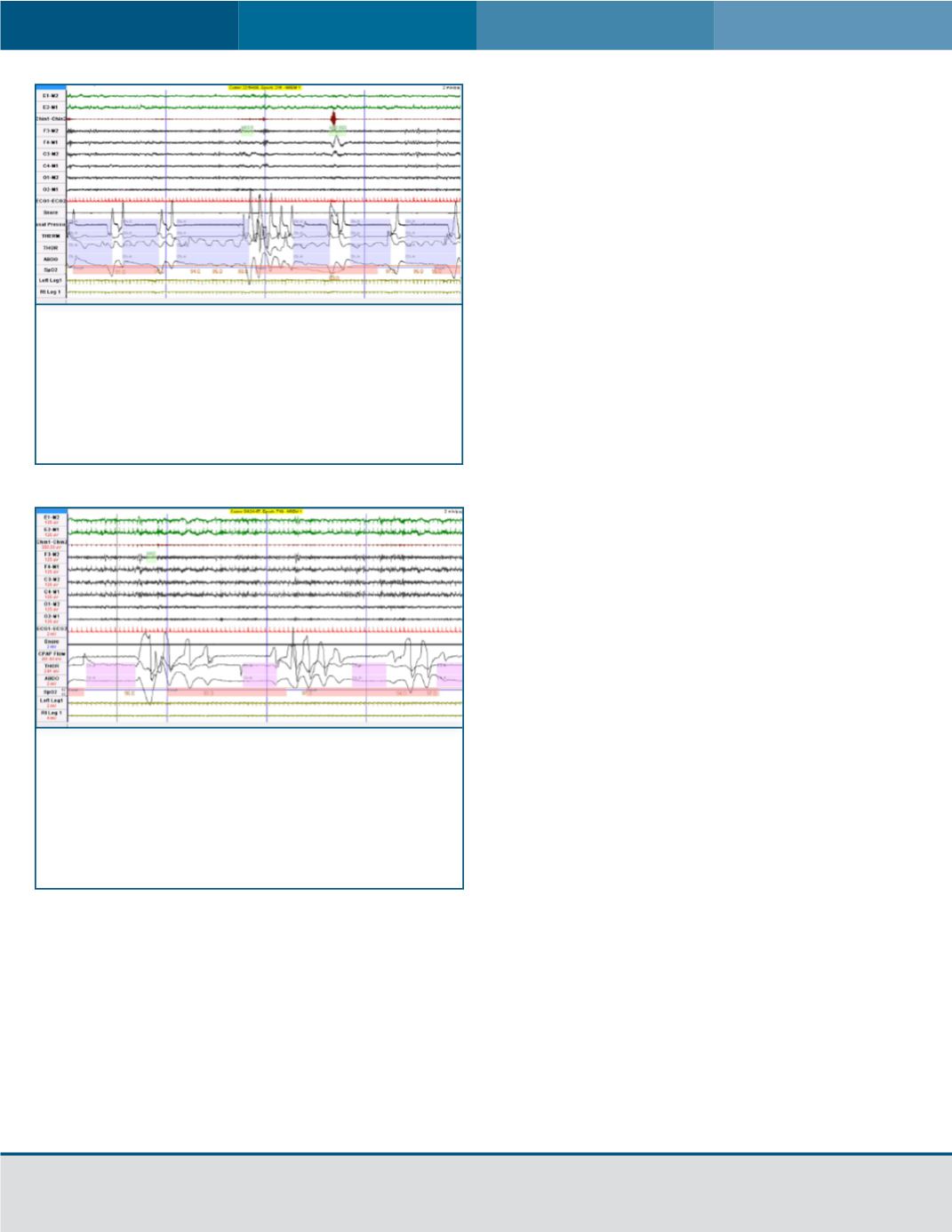
Figure 2:
Image above depicts the therapeutic portion
of the polysomnogram after the patient was initiated
on CPAP. Note that the patient now has central
apneas, characterized by an absence of flow and
a lack of respiratory effort seen in the thoracic and
abdominal belts.